What’s in a Food Label Might Surprise You
Sometimes, labeling things can be good — especially when it’s labels on the foods we choose and eat

Welcome to Health Net
University of California
UC Blue & Gold HMO from Health Net of California, Inc. (Health Net) gives you options for cost savings and access to care.

Canopy Health - Bay Area and Santa Cruz
UC Blue & Gold Bay Area and Santa Cruz members have the Canopy Health network.

Colorectal Cancer Screening Starts at 45
Regular colorectal screening helps to prevent or find cancer early when it might be easier to treat.

Preventive Care
Maintain your health and well-being with a wide range of preventive care services. No payment is required when you see your doctor for a preventive care office visit.

RealAge Test (health assessment)
The RealAge test provides you with a personalized report of your behavioral and medical health risks.

Find Social Services
Find services like food, shelter, job training, legal assistance and more. We are proud to partner with findhelp, formerly known as Aunt Bertha, to help you find programs and services in your area.

myStrength
Tools for your mind, body and spirit. Self-help resources designed to help empower you to become – and stay – mentally and physically healthy.

Healthy Baby
We have a program for pregnant and new parents. It is called Start Smart for Your Baby®

Child Anxiety
All kids deserve access to good mental health care. It's how they'll make better sense of their world.

MinuteClinic
MinuteClinic® is a convenient health care option for non-emergency illness and injuries. You can find MinuteClinics inside select CVS Pharmacy™ and Target stores.
Carousel content with slides.
A carousel is a rotating set of images, rotation stops on keyboard focus on carousel tab controls or hovering the mouse pointer over images. Use the tabs or the previous and next buttons to change the displayed slide.
Need help finding a behavioral health provider?
- For outpatient office visits, no referral is needed.
- For help, contact Customer Service – 800-663-9355 – Monday-Friday, 8:00 a.m. to 8:00 p.m. Pacific time. A Customer Service Representative will assist if you'd like help finding a provider with availability.
- Health Net will outreach to providers on your behalf and will contact you with the soonest appointment available.
Please note: routine appointments with an MD/psychiatrist may take up to 15 business days, and an appointment with a therapist may take up to 10 business days.
If you or a family member is experiencing a mental health emergency or feeling suicidal, go to the nearest ER or call 988.
Your guide to your 2024 benefits
As you're getting to know your health plan, we want to remind you of some of the highlights for 2024!
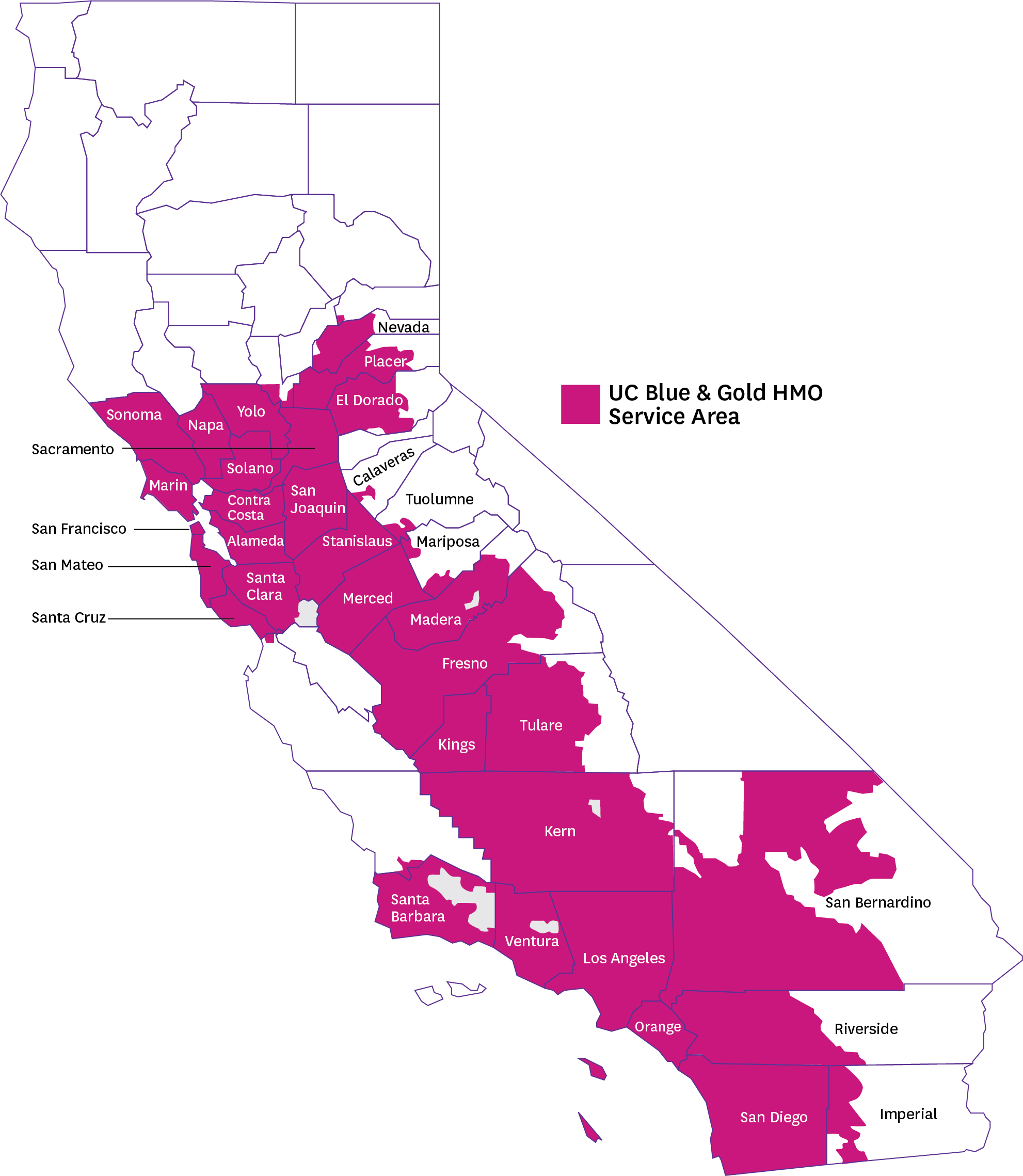
UC Blue & Gold HMO service area includes these counties:
Alameda, Calaveras, Contra Costa, El Dorado, Fresno, Imperial, Kern, Kings, Los Angeles, Madera, Marin, Mariposa, Merced, Napa, Nevada, Orange, Placer, Riverside, Sacramento, San Bernardino, San Diego, San Francisco, San Joaquin, San Mateo, Santa Barbara, Santa Clara, Santa Cruz, Solano, Sonoma, Stanislaus, Tulare, Tuolumne, Ventura, Yolo
- New for 2024! Sharecare Eat Right Now digital weight loss and diabetes prevention program.
- Reregister for an enhanced online experience. We are improving your online account experience with a new account portal and enhanced features. As a result of this upgrade, you’ll need to reregister to access your personal account. Register your member online account now!
- Get no cost adult immunizations and flu shots at Health Net pharmacies. You can continue to receive at no-cost adult immunizations, flu shots, COVID-19 vaccines and boosters at your in-network doctor's office and also at Health Net contracted pharmacies.
- Are you turning 65 and transitioning to Medicare? Learn more about the UC Medicare Choice Plan.
- 2024 UC Blue & Gold HMO plan overview
Helpful Plan Information
- The Top 10 Reasons to choose UC Blue & Gold HMO (PDF)!
- Enhanced Fertility Benefits. Fertility coverage includes IVF and ZIFT coverage at 50%, up to a lifetime limit of two treatment cycles per member.
Download your Family Planning and Maternity Guide (PDF) - Health Net Whole You – 2023 NCQA Newsletter (PDF)

