Individual & Family/Group Plans*
Coronavirus: Updates on What's Covered & More
Visit the CDC website for the most up-to-date information on COVID-19
For more information, please visit:
What is COVID-19?
COVID-19 is a disease that affects breathing. It's caused by a virus called a coronavirus, which can spread from person to person. People of all ages can get infected. Older adults and people with pre-existing medical conditions may be more likely to become gravely ill if infected.
Protect yourself and your community
We all have a role to play to help protect our families and community from the spread of COVID-19. You can follow these tips to prevent getting the virus:
- Wear a mask. Follow current state and local masking rules (PDF).
- Stay six feet apart from others if:
- they are sick;
- you are unvaccinated; or
- you are at a higher risk of getting very sick with COVID-19.
- Avoid crowds.
- Wash your hands often – at least 20 seconds each time.
- If soap and water are not available, use a hand sanitizer with at least 60% alcohol.
- Stay up to date with all vaccines including COVID-19 and flu.
Check CDC COVID-19 Community Level tool for prevention steps based on your county.
What is the COVID-19 vaccine?
A COVID-19 vaccine helps give you the best chance of keeping yourself and your loved ones safe from getting COVID-19 symptoms. And, the vaccine will help keep you from getting COVID-linked health problems in the future.
There are several COVID-19 vaccines that have been fully approved by the FDA.
For more information on COVID-19 vaccines, including safety, doses, boosters and more, see the CDC vaccine guidelines for the most current information.
You can also find vaccine information from the Advisory Committee on Immunization Practices (ACIP).
Do I have to pay for my vaccine? Or get prior approval?
Refer to your plan type below for details:
Grandfatered1 and Non-Grandfathered1 Plans
- PPO Plans:
- In-network: No cost to you. No prior approval required.
- Out-of-Network: Subject to plan's cost-share. No prior approval required.
- HDHP/HSA PPO plans:
- In-network: No cost to you. No prior approval required. Deductible waived.
- Out-of-Network: Subject to plan benefits. No prior approval required. Subject to plan deductible.
- POS Plans:
- SELECT 1 HMO tier in-network provider or SELECT 2 PPO tier in-network provider: No cost to you. No prior approval required.
- SELECT 3 tier Out-of-Network: Subject to plan benefits. No prior approval required.
- Group HMO, EOA and Salud y Más plans:
- In-network: No cost to you. No prior approval required.
- Out-of-Network: No cost to you.2 No prior approval required.
- Ambetter HMO plans (effective 4/1/24):
- In-network: No cost to you. No prior approval required.
- Out-of-Network: While your Ambetter HMO plan does not include out-of-network coverage (except for emergency and urgent care services), Health Net will cover COVID-19 vaccines received from an out-of-network provider.2 This benefit will be subject to deductible3 and a 50% coinsurance. No prior approval required. The 50% coinsurance will count towards your in-network annual out-of-pocket maximum.
1 Grandfathered plans refer to a health insurance plan that were in existence before certain provisions of the Affordable Care Act (ACA) went into effect on March 23, 2010. Non-Grandfathered plans refer to health insurance plans that are subject to all the provisions and requirements of the Affordable Care Act (ACA) since their inception.
2 If the out-of-network provider does not submit the claim on your behalf, you will need to pay out-of-pocket and submit a claim form to Health Net.
3 The in-network deductible applies to Silver 70, Bronze 60 and Minimum Coverage plans.
Do I need a doctor's script or referral prior to getting my COVID-19 vaccine at a pharmacy?
- No, you can get a COVID-19 vaccination without a doctor's script or referral at any pharmacy. Follow your health plan's guidelines for places to get other non-COVID-19 vaccines.
- You can get vaccinated at any in-network place, see the CDC vaccine guidelines for the most current information.
NOTE: Please see question "Do I have to pay for my vaccine?" for vaccine costs.
Where may I receive COVID-19 testing under my plan coverage?
You can receive COVID-19 testing at no cost from an in-network provider.
Grandfathered1 and Non-Grandfathered1 Plans
- PPO Plans:
- In-network: No cost to you. No prior approval required.
- Out-of-network: Subject to plan's cost-share. No prior approval required.
- HDHP/HSA PPO plans:
- In-network: No cost to you. No prior approval required. Subject to plan deductible.
- Out-of-network: Subject to plan benefits. No prior approval required. Subject to plan deductible.
- POS Plans:
- SELECT 1 HMO tier in-network provider or SELECT 2 PPO tier in-network provider: No cost to you. No prior approval required.
- SELECT 3 tier Out-of-Network: Subject to plan benefits. No prior approval required.
- Group HMO, EOA and Salud y Más plans:
- In-network: No cost to you. No prior approval required.
- Out-of-Network: No cost to you.2 No prior approval required.
- Ambetter HMO plans (effective 4/1/24):
- In-network: No cost to you. No prior approval required.
- Out-of-Network: While your Ambetter HMO plan does not include out-of-network coverage (except for emergency and urgent care services), Health Net will cover COVID-19 testing received from an out-of-network provider.2 This benefit will be subject to deductible3 and a 50% coinsurance. No prior approval required. The 50% coinsurance will count towards your in-network annual out-of-pocket maximum.
1 Grandfathered plans refer to a health insurance plan that were in existence before certain provisions of the Affordable Care Act (ACA) went into effect on March 23, 2010. Non-Grandfathered plans refer to health insurance plans that are subject to all the provisions and requirements of the Affordable Care Act (ACA) since their inception
2 If the out-of-network provider does not submit the claim on your behalf, you will need to pay out-of-pocket and submit a claim form to Health Net.
3 The in-network deductible applies to Silver 70, Bronze 60 and Minimum Coverage plans.
Where may I receive COVID-19 medication under my plan coverage?
You can get medication for covered services based on your plan benefits. Oral medications generally are dispensed through the pharmacy. You should refer to your Policy or Plan Contract and Evidence of Coverage for provider network and cost-share information.
Is prior approval needed for COVID-19 testing and/or medications under my plan coverage?
We will not require prior approval, prior notice and/or step therapy rules for:
- Medically-required COVID-19 diagnostic testing.
- Medical screenings.
- Medication to treat COVID-19 when ordered and/or referred by a licensed health care provider.
What are the COVID-19 Medications?
For information on COVID-19 medications, visit the CDC website.
You can also find information on COVID-19 medications on our COVID-19 Resource Center.
Can providers balance bill members for fees related to screening and testing, vaccines, or medications for COVID-19?
Balance billing is strictly prohibited by state and federal law and Health Net's PPA. Providers may not bill members for any fees related to screening and testing, vaccines, or medications for COVID-19.
How do I get an at-home COVID-19 test for free?
If you have pharmacy coverage as part of your Health Net plan, you can get an over-the-counter (OTC), FDA-approved, at-home COVID-19 test at no cost if you visit one of Health Net's in-network retail pharmacies and billed on-line to Health Net. View approved in-network pharmacy test kit list (PDF).
Get the test from the pharmacy itself. Do not get a test and pay for it at the store's normal register. If you pay for the test at the normal register, then you will need to submit a medical claim form to get reimbursed.
Visit our website to find an in-network pharmacy for your plan type.
Are there tests not covered through pharmacy?
COVID test kits that are not covered include:
- Kits that have to be sent to a lab (collection kits)
- Tests covering multiple different viruses (Combo tests)
- COVID kits obtained outside of the United States
I have a Health Net group medical plan, but the prescription coverage is through another company. How do I get an at-home COVID test for free?
Check with your pharmacy to see if they can bill your pharmacy benefit provider through their pharmacy system. You may then get an OTC at-home COVID-19 test.
You can also purchase an OTC FDA-approved, at-home COVID-19 test and be reimbursed by Health Net for the cost of the test.
Please complete and submit a Health Net medical claim form.
I bought an at-home COVID-19 test on my own, will I be reimbursed?
If you bought an OTC FDA-approved, at-home COVID-19 test at any place outside of our in-network pharmacies, a medical claim form will need to be submitted.1 You will be reimbursed as follows:
Grandfathered2 and Non-Grandfathered2 Plans
- PPO Plans:
- Subject to your plan’s out-of-network lab office visit copay.
- HDHP/HSA PPO plans:
- Subject to plan deductible and your plan’s out-of-network lab office visit copay.
- POS Plans:
- Subject to SELECT 3 tier out-of-network tier lab office visit copay.
- Group HMO, EOA and Salud y Más plans:
- No cost up to maximum.
- Ambetter HMO plans (effective 4/1/24):
- Subject to deductible3 and a 50% coinsurance.
1 Maximum of eight tests per covered member in a 30-day period. The maximum reimbursement for each test per member is $12, includes all costs such as taxes and shipping fees. A single testing kit box that includes two tests would count as two (e.g., $12 x 2 = $24)
2 Grandfathered plans refer to a health insurance plan that were in existence before certain provisions of the Affordable Care Act (ACA) went into effect on March 23, 2010. Non-Grandfathered plans refer to health insurance plans that are subject to all the provisions and requirements of the Affordable Care Act (ACA) since their inception.
3 The in-network deductible applies to Silver 70, Bronze 60 and Minimum Coverage plans.
Instructions:
- Purchase an at-home test that is on the FDA-approved list. View the FDA-approved at-home test list. Tests available without a prescription will include "OTC" (for over-the-counter at-home tests) in the Attributes column.
- Complete and submit a separate claim form for each member:
Claim form – English (PDF)
Claim form – En Español (Spanish) (PDF)
You must include a copy of your receipt. On your receipt, write or circle (if the information is on the receipt):- The name of the OTC COVID Test Kit.
- The UPC code found on the box.
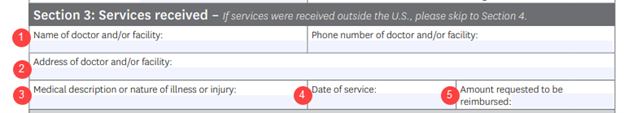
- Complete Section 1 and Section 2 of the claim form.
For Section 3, include this information in the fields as follows:- The store where you bought the test kit (Amazon, grocery store name, drug store name, etc.)
- The address of the store if applicable.
- Write "COVID-19 Home Test" and the number of tests.
- The date you purchased the kit(s).
- The amount being asked for reimbursement.
- Sign and return your claim form (don't forget the receipt).
Mail to:
Health Net, LLC
Commercial Claims
PO Box 9040
Farmington, MO 63640-9040
If you purchased a physician ordered, FDA approved test before January 15, 2022, Health Net will reimburse the member when the claim form is turned in based on what you paid.
If I bought an FDA-approved EUA at-home COVID-19 test on Amazon, how do I show my proof of purchase?
Please print an image of the digital receipt and submit it along with the claim form. If you can't provide a digital receipt, please put the order or invoice number for the purchase on the claim form. This is for proof of purchase and tracking. See above FAQ on how to be reimbursed.
Will Health Net limit the number of tests that a member can get for free?
Yes. Health Net will cover 8 OTC FDA-approved, at-home COVID-19 tests per covered member in a 30-day period. This follows California regulatory guidance effective May 12, 2023.
